As part of a project funded by the Wilhelm Sander Foundation, researchers at the Medical Faculty of the University of Duisburg-Essen have studied glioblastomas, the most aggressive brain tumors in adults, and discovered stem cells of the hematopoietic system there for the first time. The team from the DKTK partner site in Essen/Düsseldorf found that these blood stem cells promote the division of cancer cells and suppress the immune defense against the tumor. Their discovery could help develop more effective immunotherapies against brain tumors. The study was published in Nature Communications and included in Editors’ Highlights and the Cancer at Nature Portfolio.
Glioblastomas are brain tumors with a particularly severe and usually fatal course. They are usually not successfully treatable in the long term, even with the best possible surgical, chemotherapeutic and radiotherapeutic treatments. Even immunotherapies, which already achieve good results with other types of cancer, do not work. The causes are still not clearly understood, making research into the underlying mechanisms all the more important.
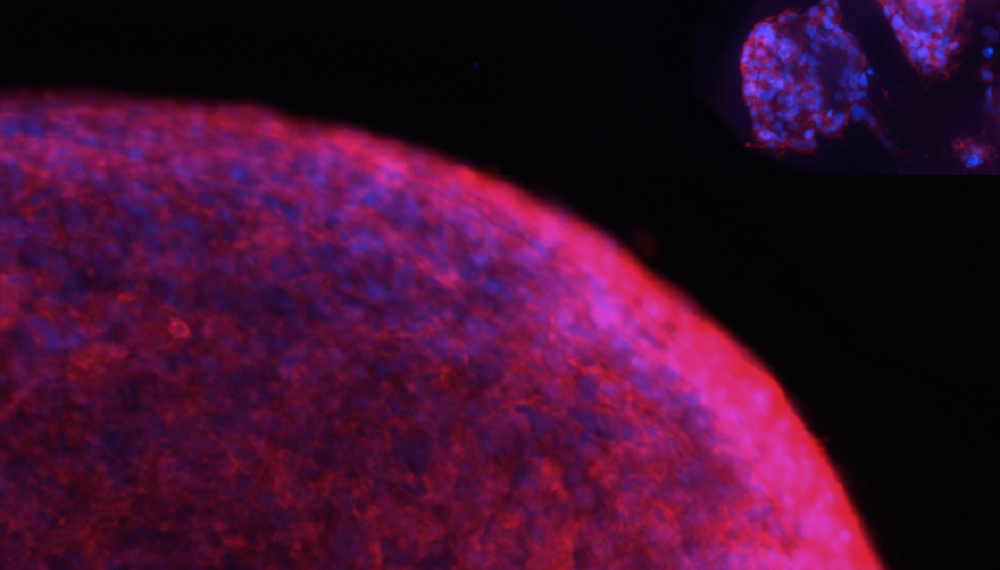
In a research project funded by the Wilhelm Sander Foundation, the team led by cancer researcher Dr. Igor Cima and Prof. Dr. Björn Scheffler, DKTK Professor of Translational Oncology at the West German Tumor Center (WTZ) of the University Hospital Essen (UK Essen), examined samples of glioblastomas and of healthy brain tissue. To their surprise, the scientists* discovered blood stem cells and precursor cells of the hematopoietic system, which are normally located in the bone marrow, for the first time in all samples of malignant brain tissue. This cell type was not detectable in healthy tissue samples.
“Glioblastomas produce immunosuppressive messengers, and in the immediate microenvironment of the tumors are found certain types of immune cells that specifically throttle the body’s own defenses. In our cell culture assay systems, hematopoietic stem cells were able to further increase the division activity of the cancer cells, while at the same time the tumor cells increased the production of the molecule PD-L1 (programmed cell death 1 ligand 1), known as an “immune brake”, on their surface.”
- Björn Scheffler
The researchers examined a total of several hundred tissue samples from glioblastoma patients. The result: the more blood stem cells a tumor contained, the more immunosuppressive messenger substances were released, the more immune-braking markers the cancer cells formed — and the lower the overall survival of those affected.
In addition, the team, in cooperation with Prof. Dr. Ulrich Sure, Director of the Clinic for Neurosurgery at the UK Essen, compared healthy with diseased cells. By sequencing the gene expression of 660 individual cells from vital tumor tissue, profiles could be generated and compared to cells from healthy bone marrow and blood. Analysis of these data reveals some new approaches to rendering the tumor-promoting cell population under study harmless in the future.
The fact that blood stem cells in the bone marrow preferentially mature into immunosuppressive cell types during the course of cancer, by being programmed accordingly by the tumor, was already known to researchers. Cancer researcher Igor Cima now suspects a similar phenomenon in glioblastoma-associated hematopoietic stem cells: “For the first time, we now see the possibility of modulating the differentiation process of glioma-associated hematopoietic stem cells in the course of further research projects — for example, by using certain cell messengers — and thus circumventing the tumor-induced immune blockade. Then immunotherapies would also have a better chance of being effective against glioblastoma.”
The research team’s findings were recently published in the prestigious journal Nature Communications and were also included in the Editors’ Hightlights in Focus Cancer and also in the cross-journal Cancer at Nature portfolio.
Wilhelm Sander Foundation: Partner of innovative cancer research
The Wilhelm Sander Foundation supported the research project with approximately 191,000 euros.
The purpose of the foundation is to promote medical research, in particular projects in the field of cancer. Since the foundation was established, a total of more than 250 million euros has been disbursed for research funding in Germany and Switzerland. This makes the Wilhelm Sander Foundation one of the most important private research foundations in Germany. It emerged from the estate of the entrepreneur of the same name, who died in 1973.
About the West German Tumor Center
At the West German Tumor Center (WTZ), patients can benefit not only from the best possible diagnostics and therapy, but also from the fact that promising approaches from laboratory research are applied in innovative clinical studies. The WTZ Center for Neurooncology unites more than 10 clinics and institutes of the University Medical Center Essen in an interdisciplinary way. Contact persons are Prof. Dr. Ulrich Sure (Director of the Department of Neurosurgery and Spine Surgery), Prof. Dr. Martin Glas (Head of the Division of Clinical Neurooncology at the Department of Neurology) and Prof. Dr. Björn Scheffler (Director of the DKFZ Department of Translational Neurooncology at the WTZ).
About the German Consortium for Translational Cancer Research (DKTK)
In the DKTK, the German Cancer Research Center (DKFZ) in Heidelberg, as the core center, joins forces on a long-term basis with university partner sites in Germany that have a particularly high reputation in oncology. With more than 3,000 employees, the DKFZ is the largest biomedical research institution in Germany. The scientists investigate how cancer develops, identify risk factors and search for new strategies to prevent people from developing cancer. They develop new methods with which tumors can be diagnosed more precisely and those affected can be treated more successfully.