One of the deadliest tumor types is pancreatic cancer . The disease is often only discovered in locally advanced or metastasized tumor stages, when surgical intervention comes too late. Researchers led by Dr. Ivonne Regel of LMU Klinikum in Munich have now gained important new insights into the causes of tumor development. They have also succeeded in defining different tumor subtypes based on differences in their metabolic programs. Funded by the Wilhelm Sander Foundation, they are thus making a significant contribution to early detection and to individualized medicine in order to improve the chances of recovery for pancreatic cancer patients.
Pancreatic ductal adenocarcinoma, also known as pancreatic cancer, is a relatively rare but particularly malignant disease. It represents the fourth leading cause of cancer-related deaths in the European Union, and only about 10 percent of patients survive the first five years after diagnosis. This is due to aggressive growth and late diagnosis of the tumor. Pancreatic cancer often manifests itself only after other organs have already been affected and metastases are present. To improve the chance of cure for pancreatic cancer patients, it is of great urgency to find new biomarkers for early detection. Another essential step is to identify tumor-specific signaling pathways that cause aggressive disease progression in order to identify new targets for therapeutic approaches.
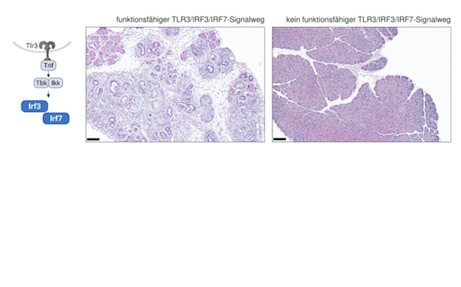
TLR3/IRF3/IRF7 signaling pathway critical for pancreatic cancer development
Pancreatic cancer development is a dynamic process involving tissue damage and inflammatory response in the pancreas. When pancreatitis occurs, the organ has a self-healing mechanism. Normal pancreatic cells can divide to replace damaged tissue. Molecules released during inflammatory and tissue-damaging processes are recognized by cell receptors, relaying signals that promote cell survival and division.
However, in pancreatic cells, this can contribute to cell degeneration and promote the development of pancreatic cancer. Researchers led by Dr. Ivonne Regel were able to show for the first time that the signaling pathway plays an important role in inflammatory responses not only in immune cells, but is also active in pancreatic cells of precursor lesions and tumor cells. This activation of the signaling pathway has an important function in pancreatic cancer development. Genetically-altered mice lacking a functional signaling pathway are unable to develop pancreatic carcinomas (see Figure). Similarly, it was genetically knocked out in pancreatic tumor cells using CRISPR/Cas9 gene scissors. These genetically modified tumor cells exhibited significantly less aggressive behavior in cell culture experiments and also showed greatly reduced metastasis in animal models.
“For the first time, we were able to demonstrate that an active signaling pathway in pancreatic cells contributes to the development of pancreatic cancer and also supports the formation of metastases.”
- Ivonne Regel
Dr. Regel’s team has made another exciting discovery: In pancreatic tumor cells, the signaling pathway surprisingly does not regulate known target genes; instead, evidence was found for epigenetic modifications. These are regulatory modifications to DNA and packaging proteins (histones) that influence the activity of genes. Thus, the current research results indicate that activation of the signaling pathway in tumor cells leads to high levels of transcription of specific tumor-promoting genes.
These genes primarily regulate tumor cell metabolism. This is particularly important because metabolites of tumor cells can be found in the blood of patients and can be used as biomarkers. “My team and I have succeeded in identifying different subtypes of pancreatic cancer from the blood of cancer patients based on differences in their metabolic programs” said Dr. Regel. “In further studies, we now want to find out to what extent the development of pancreatic cancer subtypes is regulated by the signaling pathway.”